Impact of tumor microenvironment on tumor resistance and its role in shaping tumor plasticity and stroma reactivity
This group belongs to the UMR 1186 - Integrative tumor immunology and immunotherapy
Cancer immunotherapy is currently of great interest for patients with advanced cancer. Its goal is to boost the immune response against tumor cells that use multiple resistance strategies to neutralize and paralyze the host’s immune system. Even if these innovative treatments have improved the survival of some patients, the response rate remains limited due to multiple mechanisms of resistance and immune tolerance. Our objective is to better understand the role of the microenvironment in which the tumor develops on the sensitivity/resistance of tumor cells to this type of treatment.
Research topics
Our research program relies on various points aiming to better characterize the key role of the tumor microenvironment (TME) and the p53 tumor suppressor in the regulation of the anti-tumor cytotoxic T response.
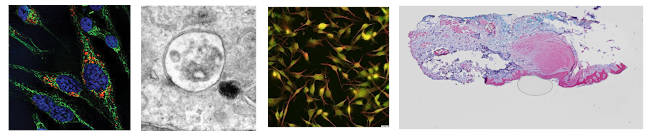
In particular, we endeavor to elucidate the influence of hypoxia, epithelial-mesenchymal transition (EMT) and tumor-associated fibroblasts (CAF) on tumor plasticity, resistance to immune surveillance and response to immunotherapy. Our work also concerns the analysis of the molecular mechanisms associated with the emergence of resistant tumor variants, in particular linked with the Axl receptor or with EMT-associated the transcription factors. Our research program also aims to determine the impact of mutations in the gene encoding the tumor suppressor protein p53 on the anti-tumor cytotoxic response and on the expression of immune checkpoint ligands, and therefore on the response to immunotherapy targeting immune checkpoints.
In addition to this cognitive research, we are also developing translational research programs aiming to develop 3D culture models in order to better characterize the impact of EMT on resistance to treatments and on the immune response, as well as its implication in recurrent breast tumors. This program also aims to design high-throughput (microfluidic) screening methods to analyze the impact of EMT on immune interactions during the progression of breast carcinoma and on resistance to immunotherapy. Finally, we are developing a translational research program in kidney cancer aiming at highlighting the possible relationships between mutations in the VHL gene (associated with pseudo-hypoxia) and tumor resistance to immunotherapy targeting PD-1.
The aim of our program is thus to make new advances in the understanding of cellular and molecular mechanisms associated with tumor resistance to immunosurveillance and immunotherapies targeting immune checkpoints, in order to identify new therapeutic targets and to develop more effective combined strategies.